Introduction
This is an introductory guide for those who experience long-term shortness
of breath and want to manage it better. People close to them may also find it useful. Breathlessness can be distressing, it is both a physical and an emotional experience that can effect and reduce quality of life.
I am not sad. I just feel down – breathing does that to you."
If this is something you are struggling with then this guide may be for you. We do not have a magic wand but find that a little knowledge goes a long way in helping to be able to take control and achieve the things in life that really matter.
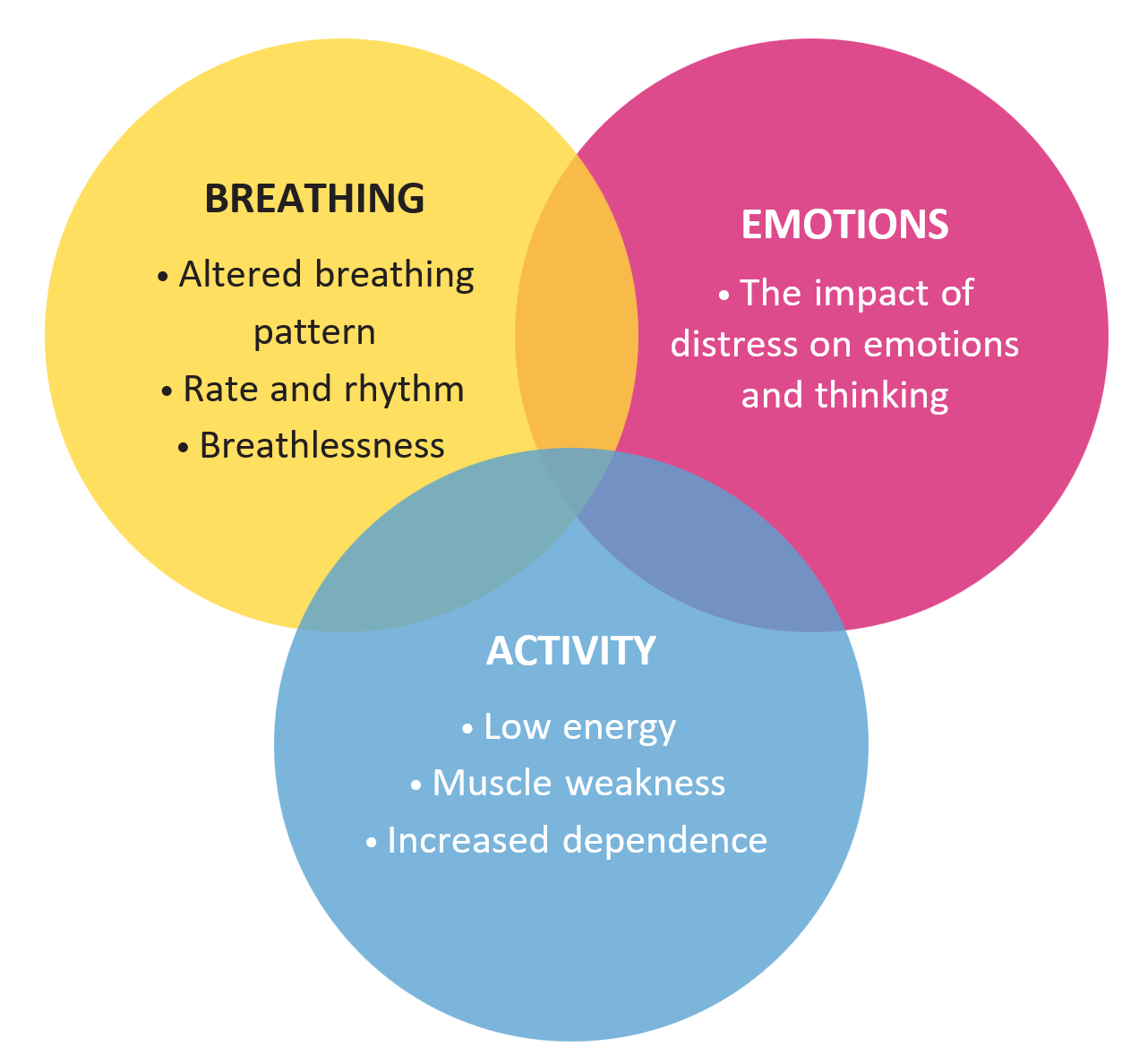
Understanding the influencing components of breathlessness
Breathing pattern – rate and rhythm
How your lungs work
Oxygen is a gas in the air that the body needs in order to function. The lungs are the organs that take oxygen into the body.
Lungs are located in the chest, one either side of the heart. The inside of the lung looks like a giant sponge with a mass of fine tubes, the smallest of which end in tiny air sacs called alveoli. When you breathe in, the air flows through your mouth or nose and down the series of tubes until it reaches the alveoli, where the oxygen enters the blood through tiny vessels called capillaries.
Carbon dioxide (CO2), a waste product from the cells, is passed out of the blood and is breathed out when you exhale.
Under the lungs is a large muscular sheet, called the diaphragm, which separates the chest cavity from the abdomen. The diaphragm is the main muscle of breathing and assists the movement of air in and out of the lungs. It is a very energy efficient muscle.

Natural responses
You may have found that when you feel short of breath one or more of the following might happen.
Your shoulders and upper chest muscles work harder
We usually use the very efficient diaphragm and lower chest muscles to breathe. In heavy exercise the muscles of the upper chest and shoulders can help, but these muscles are not designed to work for long periods of time and get tired easily. If overworked the muscles become tense, work less efficiently and use more oxygen – adding to the sense of breathlessness.
The rate of breathing increases
Taking rapid shallow breaths may feel helpful for a short period of time. Unfortunately, breathing this way for a longer period is inefficient. It takes more effort and therefore more energy to bring air in quickly (think of trying to blow up a balloon quickly rather than gently). Oxygen is not available to the body until it reaches the alveoli (air sacs). If it does not have time to reach them because you are already breathing out, the body cannot use the oxygen that is brought in.
Breaths become deeper
We normally take twice as long to breathe out as to breathe in. When breathless, often the instinct is to always concentrate on trying to take a deep breath in. This does not allow time for air already ‘used’, rich in carbon dioxide, to be breathed out.
Working to challenge these natural responses is often helpful when trying to control breathlessness.
The impact of distress
Feelings of fear, anxiety, frustration, anger, panic and unrest are common responses when experiencing shortness of breath. They are a protective reaction by your body, similar to when something causes you pain.
These emotional reactions can have a direct effect of increasing the heart and breathing rate as well as alerting your body (as when you are startled), which results in tensing muscles. When this happens, the feeling of breathlessness is stronger, which in turn leads to more anxiety and even panic.
Distress and avoidance
It is natural to avoid activities and situations associated with distressing experiences of breathlessness, low energy and loss of control in order to gain relief. Unfortunately, when this becomes a habitual way to gain relief it may lead to a loss in confidence and for leg muscles to weaken and become deconditioned. This reduced confidence and physical fitness leads to an increase in breathlessness.
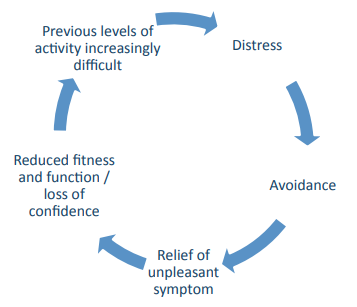
Deconditioning – the hidden menace
This is a term for weakness in muscle strength and a reduction of muscle size following a period of inactivity. It is most noticeable in the leg muscles, making standing up from a seated position and/or climbing stairs difficult to do without using your arms to help. Deconditioned muscles can make a person feel weak and tired, often masquerading as disease progression. The good news is that, targeted in the right way, it is reversible.
Natural compensation behaviours
It is natural to change the way we do things in order to find relief from distressing symptoms.
Here are some of the common compensation behaviours you may recognise:
- Breathing deeply and quickly to get more breath in
- Rushing from place to place, and to sit down quickly to ‘beat the breathlessness’
- Using your arms to pull strongly on the banister rail to help with climbing the stairs rather than letting your legs do the work
- Pushing up strongly with the arms when standing up from a chair and tending to sit down heavily rather than controlling the speed with your leg muscles
- Only exercising your legs by walking, avoiding other activities that are hard
- Being active and only stopping when feeling exhausted rather than a little tired
Although they may give short-term relief, these behaviours may lead tolong-term negative effects. Challenging them may be of benefit.
In control for what matters
Learning to be in control of your breathing, your emotions and your physical activities can lead to an improved quality of life. It is worth taking the time to think about what matters to you – these are the things that are worth the effort when working on achieving them.
The principle of small gains
When you make small differences and achievements, these are added together; their total has the potential to improve quality of life.
You may be able to achieve this by:
- Controlling your breathing rate and rhythm
- Becoming oxygen and energy efficient
- Controlling your thinking and emotions
- Knowing you are not alone in experiencing distressing breathlessness and low energy
- Retaining or regaining physical fitness
- Retaining or regaining independence
- Learning to relax and enjoy life.
The Breathlessness Service
If you have a life-limiting illness and are interested in learning more about managing your breathlessness in the way we describe, we may be able to help.
What we offer:
- A member of the Breathlessness Management Team will discuss your symptoms of breathlessness and low energy and how they affect your everyday quality of life and independence
- They will explore how to achieve your main aims in everyday life, learning a wide variety of techniques to help you to help yourself
- You will receive 1-3 sessions of approximately one hour, depending on your particular needs
- The service is based in both the Taunton and Yeovil Hospice hubs. We can visit you if you are unable to leave your home
Referral to St Margaret’s
Your healthcare professional (e.g. GP, consultant, specialist nurse) can refer you to our service. These are the questions they will need to tell us the answers to:
- How your breathlessness causes you trouble and distress?
- What would you like to be able to achieve?
- What other teams are/have been involved in your care for breathlessness symptoms?

